What Exactly is Happening in Your Body?
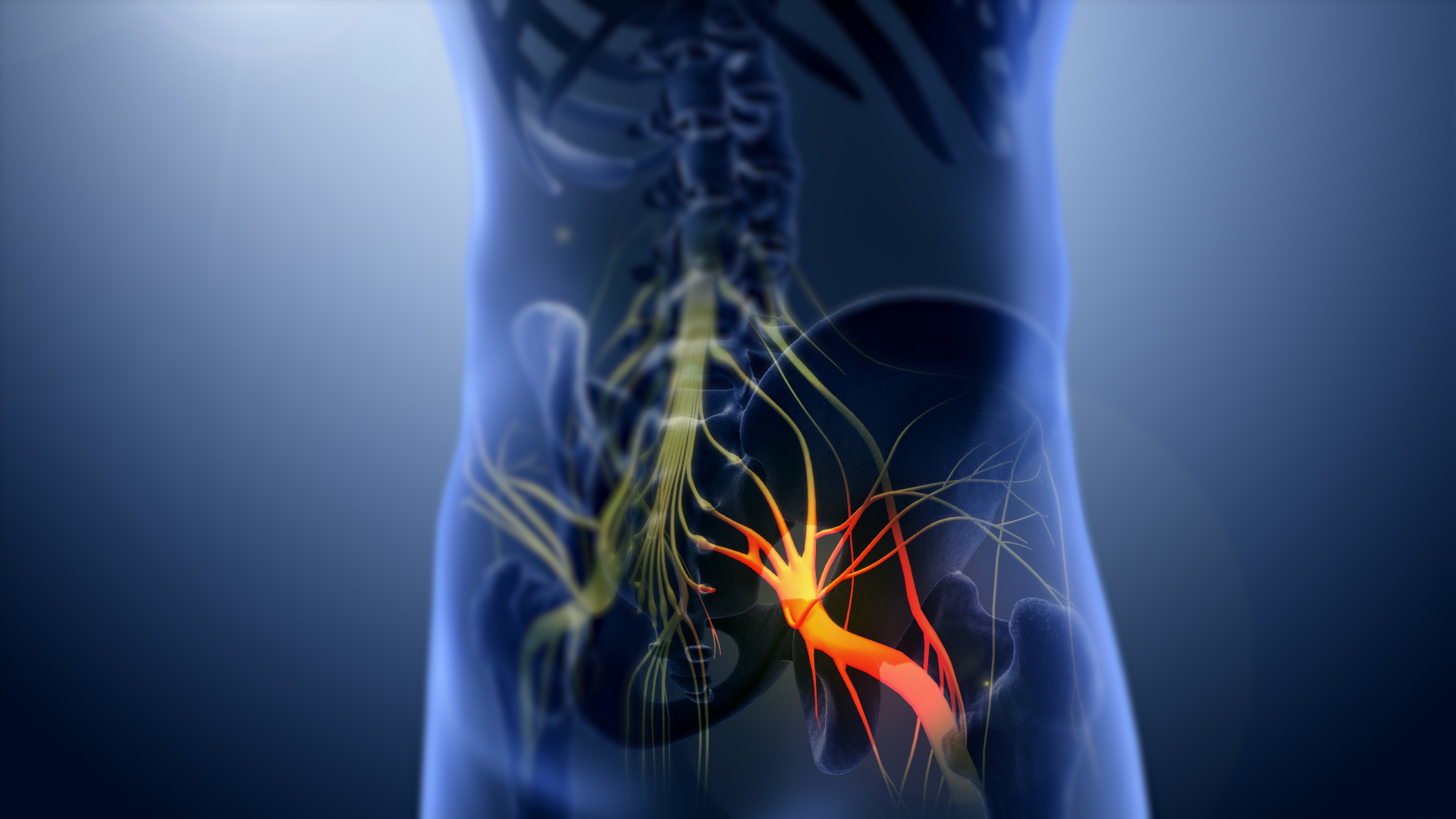
Your sciatic nerve is the longest and thickest nerve in your body - about as wide as your thumb in some places. When this nerve gets irritated or compressed, it sends pain signals along its entire pathway. Sciatica isn't actually a diagnosis itself, but rather a symptom of an underlying problem affecting this important nerve. Let's explore what this means for you in practical terms.
Detailed Symptoms: What You Might Experience
Pain Characteristics:

- A sharp, electric shock-like sensation
- Pain that's typically worse in the leg than in the back
- Discomfort that follows a predictable path (buttock to thigh to calf)
- Pain levels that fluctuate based on position and activity
What makes the pain worse?
- Sitting for long periods (especially on soft couches)
- Sudden movements like coughing or sneezing
- Bending forward or twisting of the back
- Extended periods of standing
- Carrying heavy objects
Underlying Causes: What's Irritating Your Sciatic Nerve?

1. Lumbar Herniated Disc (Most Common):
The jelly-like center of a spinal disc leaks out. This material presses directly on nerve roots causing irritation.

2. Degenerative Disc Disease:
Natural aging causes discs to lose hydration, resulting in reduced disc height and more friction. This can cause spurs to develop, impinging on the nerves.

3. Spinal Stenosis:
Narrowing of the spinal canal. This is particularly problematic when bending backward and is more common in the elderly.
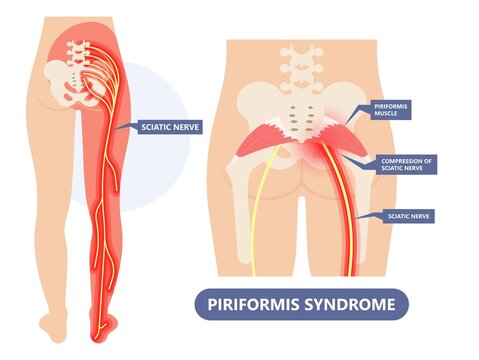
4. Piriformis Syndrome:
The sciatic nerve runs directly beneath the piriformis muscle. When this muscle spasms, it causes irritation and pain running down the nerve.

5. Spondylolisthesis:
One vertebra slips forward over another, creating instability and nerve compression. This may develop gradually or after injury.
Diagnosis: What to Expect at the Doctor's

Your healthcare provider will likely:
1. Take a Detailed History
Your doctor will ask about your symptoms, their onset, and what makes them better or worse.
2. Perform Physical Examination
- Straight leg raise test
- Muscle strength assessment
- Reflex testing
- Sensory evaluation
3. Order Imaging (If Needed)
- X-rays: To check bone alignment and look for bone spurs.
- MRI: The best imaging for soft tissue details, especially useful for disc issues.
- CT scan: An alternative if MRI is not possible or contraindicated.
- EMG (Electromyography): For suspected nerve damage and to differentiate between nerve root and peripheral nerve issues.
Comprehensive Treatment Approaches

First-Line Conservative Treatments:
- Activity Modification: Learning movement patterns that reduce irritation on the sciatic nerve.
- Targeted Physical Therapy: Typically 2-3 sessions per week initially, focusing on strengthening and stretching.
- Medication Management:
- NSAIDs (ibuprofen, naproxen) for inflammation.
- Muscle relaxants for spasms.
- Neuropathic agents (gabapentin) for nerve pain.
- Short-term oral steroids for severe cases to reduce inflammation.
- Home Remedies:
- Ice packs (acute phase) to reduce swelling and pain.
- Heating pads (chronic stiffness) to relax muscles and improve blood flow.
- Lumbar support cushions for better posture while sitting.

Interventional Options:
- Epidural Steroid Injections: Delivers anti-inflammatory medicine directly to the affected area around the nerve roots.
- Nerve Root Blocks: More targeted injections that focus on a specific nerve root causing pain.
- Radiofrequency Ablation: For chronic cases, especially if pain is due to facet joint arthritis; uses heat to deactivate nerve fibers.
Practical Self-Care Strategies
Movement Tips:
- Walk short distances frequently to keep the spine mobile.
- Avoid both prolonged sitting and standing; alternate positions often.
- Sleep in the fetal position with a pillow between your knees to align your spine.
- Use your legs (not your back) when lifting objects to protect your spine.
Workplace Adjustments:
- Set your computer monitor at eye level to prevent neck strain.
- Use a footrest if needed to maintain proper posture.
- Take micro-breaks every 30 minutes to stand up and take short walks.
- Consider a sit-stand workstation to vary your posture throughout the day.
Helpful Exercises:
- Gentle knee-to-chest stretches to decompress the lower back.
- Pelvic tilts to mobilize the lower back and strengthen core muscles.
- Piriformis stretches (seated figure-4) to release tension in the piriformis muscle.
- Core stabilization exercises to support the spine and prevent future episodes.
When to Seek Immediate Care
Contact your doctor right away or go to the ER immediately if you notice:
- Sudden severe weakness in your leg or foot.
- Numbness in the "saddle area" (groin and inner thighs).
- Loss of bladder or bowel control.
- Pain that keeps worsening despite rest and conservative measures.
Prevention: Keeping Your Back Healthy
- Maintain strong core muscles through regular exercise.
- Practice proper posture, especially when sitting or lifting.
- Stay active with low-impact exercises like swimming or walking.
- Use lumbar support when driving or sitting for extended periods.
- Manage stress, as tension can worsen muscle tightness and pain.
Living Well With Sciatica
While sciatica can be incredibly painful, remember:
- It's rarely permanently damaging.
- Most cases resolve with time and proper care.
- You have multiple treatment options available.
- Small daily adjustments can make a big difference in managing your symptoms.