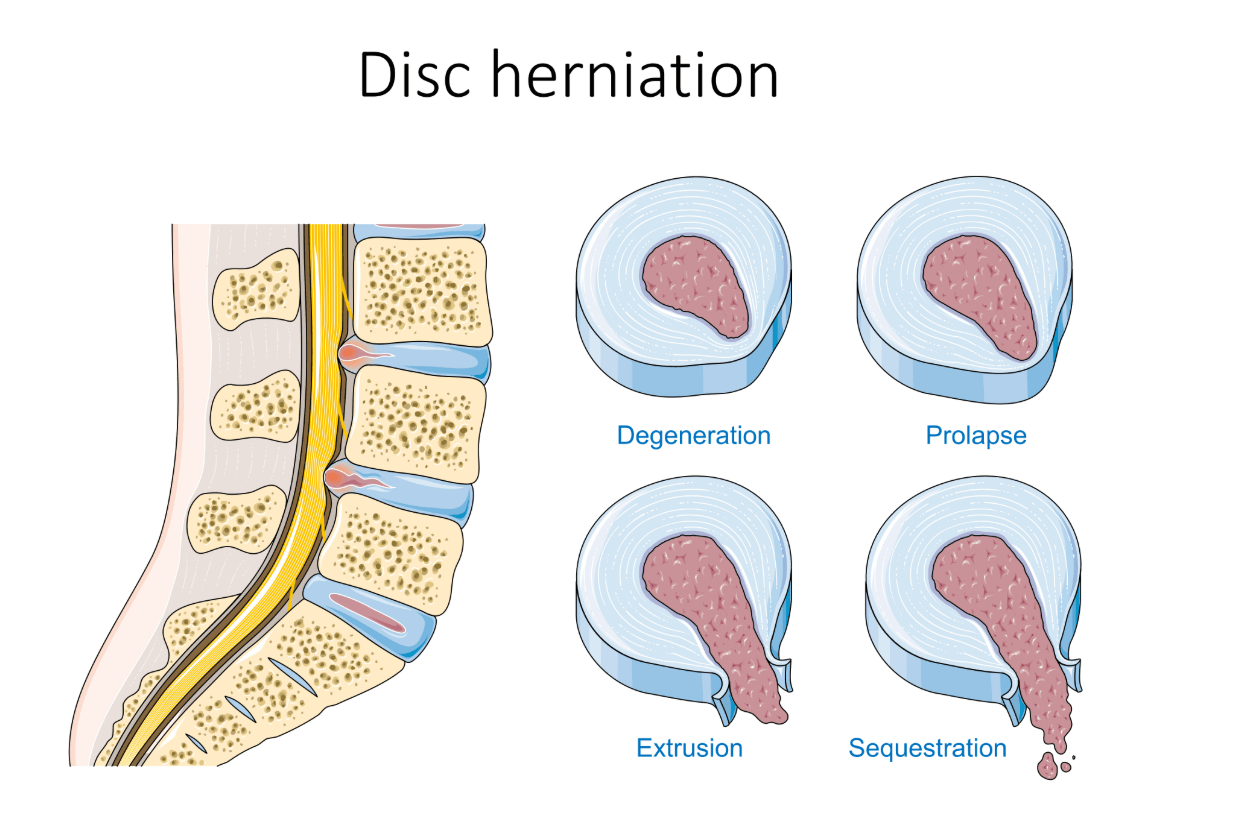
What is a Herniated Lumbar Disc?
The spine is made up of bones (vertebrae) cushioned by spinal discs, which act as shock absorbers. A herniation occurs when the disc’s tough outer layer tears, allowing the soft inner gel to leak out. This can press on spinal nerves, causing pain, numbness, or weakness (often called sciatica if it affects the sciatic nerve).
Common Symptoms
- Localized Pain: Dull or sharp pain in the lower back.
- Radiating Pain: Down the buttock, thigh, calf, or foot.
- Numbness/Tingling: "Pins and needles" in the leg or foot.
- Muscle Weakness: Foot drop or difficulty standing on toes.
- Worsening Pain: With sitting, bending, or coughing.
Causes & Risk Factors
- Age: Discs dry and weaken over time.
- Injury: Heavy lifting, twisting, or trauma (e.g., car accidents).
- Lifestyle: Smoking, obesity, and sedentary jobs increase risk.
Diagnosis
- History and physical exam (reflexes, strength, straight-leg raise test).
- MRI: Best for visualizing discs and nerves.
- CT Myelogram: Alternative to MRI.
- X-ray: Rules out fractures or arthritis.
Treatment Options
Non-Surgical Treatments
- Short rest (1–2 days), gradual activity return.
- NSAIDs, oral steroids, or epidural injections.
- Physical therapy: core exercises, McKenzie stretches, hamstring stretches.
Surgical Options
- Microdiscectomy: Minimally invasive disc removal.
- Laminectomy: Bone removal to relieve pressure.
Recovery & Prevention
- Most recover within 6 weeks with proper care.
- Posture: Use lumbar support, sit/stand properly.
- Lifting: Use legs, avoid twisting motions.
- Exercise: Walking, swimming, low-impact movement.
FAQs
- Will the disc heal on its own? Yes, the body can absorb the gel over time.
- Can it come back after surgery? Yes (~5–10% risk), but precautions help.
- Is surgery always needed? No—most recover without it.