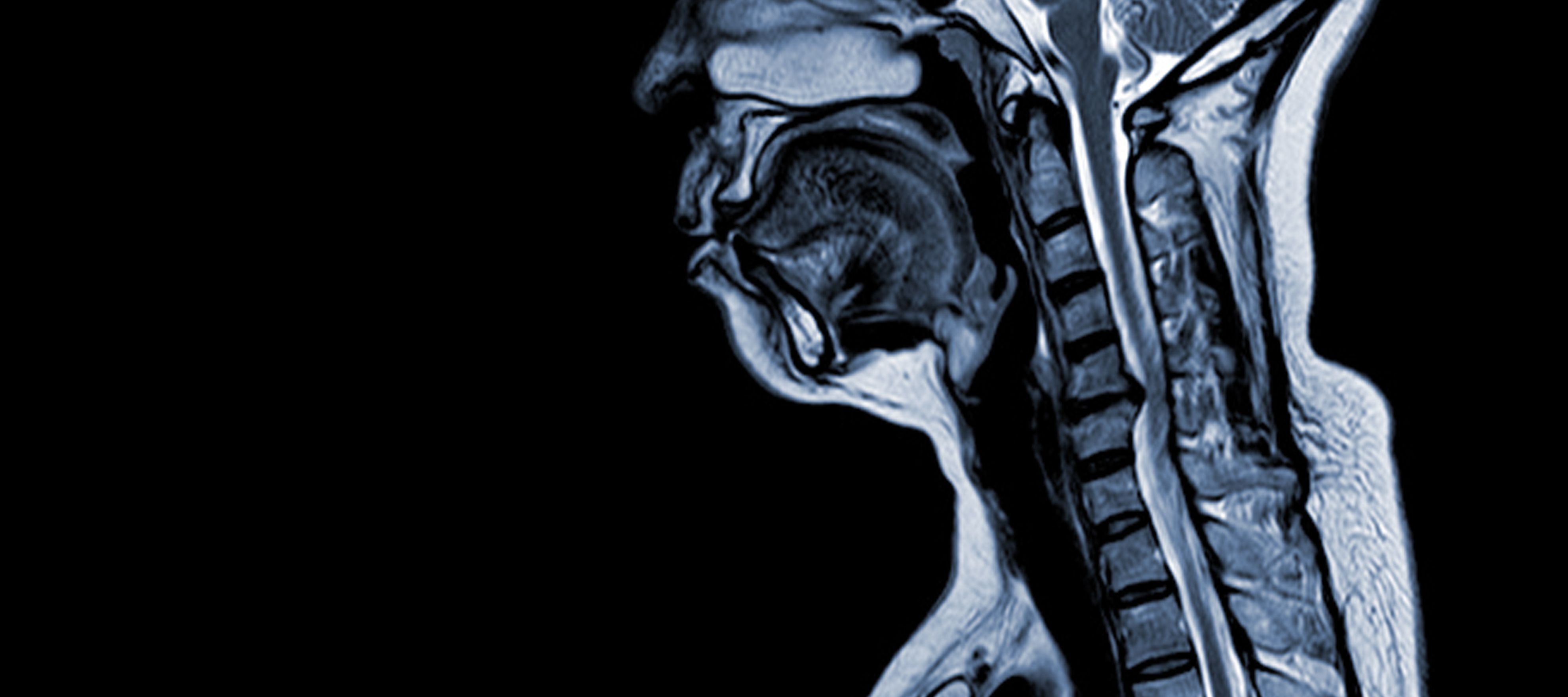
What Exactly is Cervical Myelopathy?
Think of your spinal cord as the body's main information highway - a thick bundle of nerves sending messages between your brain and the rest of your body. When this crucial pathway gets squeezed in your neck area (the cervical spine), it's like putting a kink in a garden hose. The flow of nerve signals gets disrupted, leading to various symptoms collectively termed "myelopathy."


Why Your Neck is Vulnerable
Your cervical spine has seven small, stacked bones (vertebrae) with:
- Shock-absorbing discs between them
- Flexible joints that allow movement
- A central tunnel (spinal canal) protecting the cord
Over time, these structures can change and narrow the canal, putting pressure on the spinal cord itself rather than just single nerves.
Detailed Causes: What's Squeezing Your Spinal Cord?
1. The Aging Process (Most Common Cause)
- Disc Degeneration: As discs dry out with age, they bulge outward causing pressure on the spinal cord.
- Bone Spurs: Extra bone growth around joints
- Thickened Ligaments: Spinal ligaments can stiffen and bulge inward

2. Structural Problems
- Herniated Discs: When disc material pushes into the spinal canal
- Congenital Stenosis: Some people are born with a narrower canal
- Spondylolisthesis: When vertebrae slip out of alignment

3. Other Causes
- Trauma: Car accidents or falls that fracture vertebrae
- Tumors: Abnormal growths pressing on the cord
- Inflammation: From conditions like rheumatoid arthritis
Symptoms: What You Might Experience
Early Warning Signs

Hand Changes:
- Difficulty with fine motor skills (writing, buttoning shirts)
- Frequent dropping of objects
- Numbness or "electric shock" sensations

Walking Problems:
- Feeling unsteady, especially in dim light
- Legs feeling heavy or stiff
- Needing to watch your feet while walking
As It Progresses
- Loss of Dexterity: Trouble with keys, zippers, or utensils
- Muscle Weakness: Especially in hands and arms
- Bowel/Bladder Issues: (In severe cases) urgency or retention
What Makes It Better/Worse
- ✔️ Often improves with rest
- ✖️ Typically worsens with neck extension (looking up)
- ⚠️ Symptoms may come and go at first
Diagnosis: How Doctors Figure It Out

The Examination
Your doctor will check:
- Reflexes (often exaggerated in myelopathy)
- Hand Function (finger dexterity tests)
- Balance and Gait (walking pattern)
- Sensation (with light touch or pinprick)
Key Diagnostic Tests
- MRI Scan - The gold standard showing cord compression
- X-rays - To assess spinal alignment and degeneration
- EMG/NCS - Rules out peripheral nerve problems
Treatment Options Explained

Non-Surgical Management
(For mild cases or patients who can't have surgery)
Physical Therapy:
Focuses on neck stabilization
Medications:
- NSAIDs for inflammation
- Neuropathic pain drugs (like gabapentin)
- Short-term steroids for flare-ups
Lifestyle Modifications:
- Neck collar for temporary support
- Home safety adjustments
- Activity modification
Surgical Treatments
(When cord compression needs direct relief)

Anterior (Front) Approaches
(A small cut is made through the skin of the front part of your neck)
- ACDF: Removes problematic disc and fuses vertebrae
- Corpectomy: Removes entire vertebra body for severe stenosis
Posterior (Back) Approaches
- Laminectomy: Creates space by removing bone
- Laminoplasty: Hinges bone open to make more room for your neck
Recovery Timeline

- Hospital Stay: Typically 1-3 days
- Initial Recovery: 2-6 weeks for basic healing
- Full Recovery: 3-12 months for nerve improvement
- Physiotherapy: Usually starts at 6 weeks after surgery
Living With Cervical Myelopathy
Daily Life Adjustments
- Kitchen Tools: Use built-up handles
- Dressing: Choose Velcro over buttons
- Bathroom: Install grab bars
- Walking Aids: Consider canes or walkers if unsteady
What to Avoid
- High-impact activities
- Chiropractic neck manipulations
- Prolonged neck positions (like looking up at stars)
Monitoring Your Condition
Keep a symptom diary tracking:
- Hand function changes
- Walking endurance
- New symptoms
- Medication effects
Prevention and Long-Term Outlook
Slowing Progression
- Posture Awareness: Keep ears aligned with shoulders
- Neck Strengthening: Under professional guidance
- Bone Health: Adequate calcium/vitamin D
- Regular Check-ups: Especially if symptoms change
Prognosis Factors
- Better outcomes with earlier treatment
- Some nerve damage may be permanent
- Most patients stabilize or improve with proper care
When to Seek Emergency Care
Go to the ER immediately if you develop:
- Sudden severe weakness
- Loss of bladder/bowel control
- Rapid symptom worsening
- After significant neck trauma