Understanding Cervical Disc Arthroplasty
Cervical disc arthroplasty is an advanced surgical procedure that replaces a damaged intervertebral disc in your neck with an artificial implant while preserving natural motion. Unlike traditional spinal fusion, this innovative treatment maintains your spine's flexibility while relieving pain caused by nerve compression. It's particularly beneficial for patients with degenerative disc disease who want to maintain neck mobility.

Key Features of the Procedure
- Motion-preserving technology: Maintains natural neck movement unlike fusion
- Minimally invasive approach: 3-5 cm incision along natural neck creases
- Efficient procedure: Typically takes 1-2 hours under general anesthesia
- Precise placement: X-ray guided positioning of artificial disc
- Modern closure: Absorbable sutures or surgical glue
Step-by-Step Surgical Process
1. Anesthesia
General anesthesia will be administered; you will be asleep during the entire procedure.
2. Positioning
Supine position with neck slightly extended for optimal access.
3. Approach
3-5 cm horizontal incision along natural neck creases with careful separation of tissues.
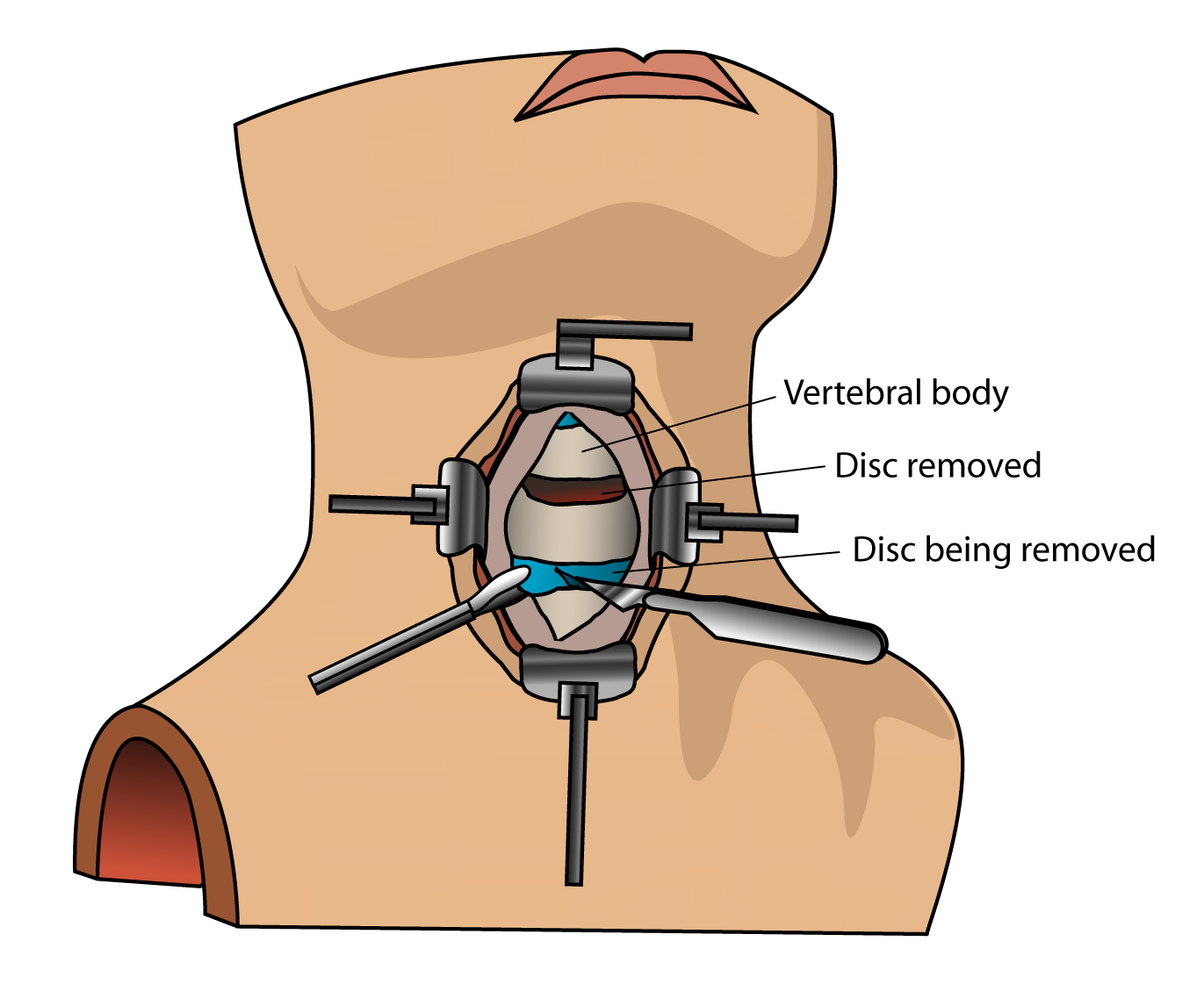
4. Disc Removal
Complete removal of damaged disc material and decompression of nerve roots.
5. Implant Placement
Precise sizing and positioning of artificial disc guided by X-rays.
6. Closure
Skin closed with absorbable sutures or surgical glue.
Comprehensive Recovery Timeline
Immediate Postoperative Period
(First 24 Hours)
- Monitoring in recovery area
- Pain management with IV/oral medications
- Encouraged to walk same day or next morning
- Possible temporary sore throat or swallowing discomfort
First Week After Surgery
- Oral pain medications as needed
- Daily incision care
- Gradual return to light activities
- Follow-up appointment at day 10
Long-Term Recovery
(6 weeks - 12 Months)
- Full integration of artificial disc
- Gradual return to all normal activities
- Physiotherapy typically starts after 6 weeks
- Final evaluation of surgical outcomes
Arthroplasty vs. Fusion: Key Differences
Advantages of Disc Replacement
- Preserves natural neck motion
- Lower risk of adjacent segment degeneration
- No bone graft required
- Faster recovery timeline
- Reduced long-term stiffness
When Fusion Might Be Preferred
- Multi-level degeneration
- Significant facet joint arthritis
- Spinal instability or deformity
- Certain autoimmune conditions
Potential Risks and Complications
- Infection: Superficial or deep
- Bleeding: Hematoma formation
- Nerve injury: Nerve root or spinal cord
- Implant issues: Failure or malposition
- Dysphagia: Temporary swallowing difficulties
- Adjacent segment disease: Though less common than with fusion
Activity Guidelines After Surgery
Recommended Progression:
- First 2 Weeks: Light walking, avoid heavy lifting
- Weeks 3-6: Gradual increase in activity, gentle stretching
- After 6 Weeks: Typically cleared for most activities
- 3+ Months: May return to sports/impact activities
Permanent Considerations:
- Maintain good neck posture
- Regular exercise to strengthen supporting muscles
- Avoid tobacco products (impairs healing)
- Periodic follow-up imaging as recommended
When to Seek Immediate Care
Contact your surgical team immediately if you experience:
- Sudden severe neck pain
- Progressive weakness in arms/hands
- Difficulty breathing/swallowing
- Fever over 37.5°C
- Unusual drainage from incision
- New or worsening neurological symptoms
Long-Term Outlook
Cervical disc arthroplasty offers excellent outcomes for properly selected patients:
- 90% of patients report significant pain relief
- 85-90% maintain normal range of motion
- Lower reoperation rates compared to fusion
- Most patients return to normal activities within 3 months
- Long-term studies show durable results at 10+ years